Respiratory Viral Determinants of Chronic Lung Allograft Dysfunction (RVI in CLAD)
Principal Investigators: Cynthia Fisher, MD MPH and Erika Lease, MD
Study Design: Two-center, prospective, longitudinal cohort study
Study Sponsors: Investigator Initiated
Respiratory viruses in particular can lead to serious illness and complications in lung transplant recipients. This study aims to understand how these viruses affect the graft function and hopes to provide valuable data to help with their management in this patient population.
Background
In the case of lung transplant recipients, contraction of respiratory viruses may potentially cause a form of post-transplant disease called chronic lung allograft dysfunction (CLAD). Long-term outcomes of lung transplantation are significantly worse than for all other organ transplants, primarily due to CLAD, which affects approximately 50% of lung transplant recipients (LTR) by 5 years post-transplant. Despite the importance of CLAD as a major contributor to lung graft failure, diagnosis is difficult and subjective, and the pathogenesis is incompletely understood.
Multiple studies have indicated RVI as an independent risk factor for the development of CLAD. However, there are no large prospective studies of RVI in lung transplant patients that use longitudinal sampling with sensitive and quantitative methods to systematically examine the detailed virologic characteristics of RVI and how they relate to CLAD
This is a two-center, prospective, longitudinal cohort study of adult LTR with symptomatic lower respiratory tract RVI where the aim is to-
Help us better understand how respiratory viruses affect lung transplant patients
Provide valuable information about the clinical course of respiratory viral infections
Provide important insight into how we can prevent complications after lung transplant
Study Design
In this two-center, prospective, longitudinal cohort study of adult LTR with symptomatic lower respiratory tract RVI, the plan is to enroll a total of 100 LTR from both sites over 3 years.
Hypothesis
In LTR with symptomatic RVI, specific viral and host factors will predict early decline in FEV1 following RVI.
Specific viral and host parameters determine the risk for CLAD in LTR with symptomatic RVI.
Early decline in FEV1 after symptomatic RVI will predict risk of CLAD
Outcomes
Characterize viral factors that impact early FEV1 changes in LTR with symptomatic RVI by characterizing the detailed viral kinetics of symptomatic RVI in LTR, defining the course of early FEV1 changes after symptomatic RVI in LTR, and analyzing the association between virologic and host parameters and early FEV1 changes after symptomatic RVI in LTR.
Characterize viral and host determinants of CLAD in LTR with symptomatic RVI.
Analyze the association between early decline in FEV1 after symptomatic RVI and subsequent development of CLAD.
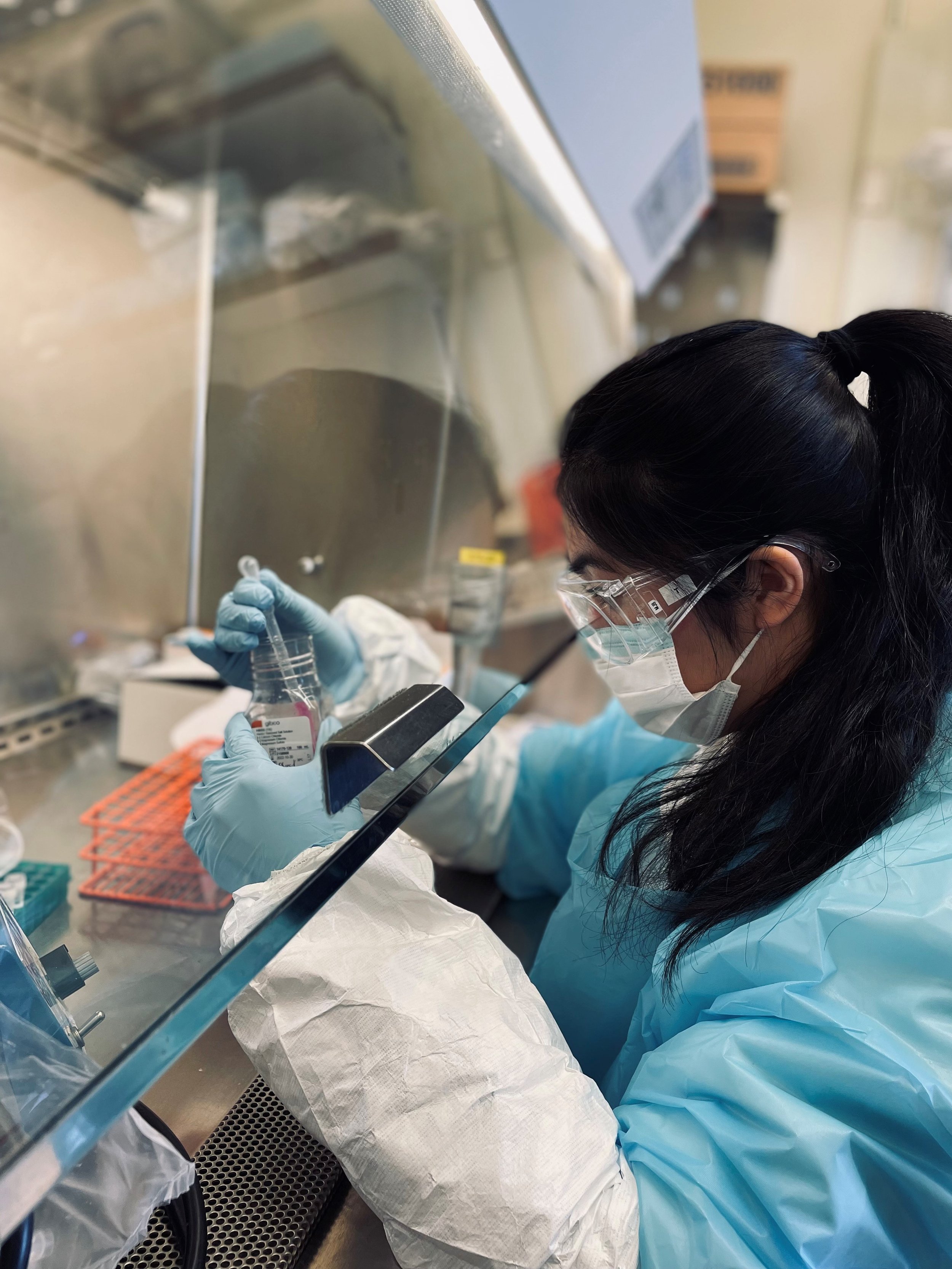
At both sites, LTR who have symptoms of lower tract infection and/or exhibit a decline in spirometry typically undergo diagnostic bronchoalveolar lavage (BAL), on which an extended respiratory viral PCR panel is routinely sent. Eligible patients who test positive for a respiratory virus will be approached for enrollment and informed consent. After consent, patients will be trained on nasal swab self-collection techniques. They will then perform nasal swabs and record home spirometry values via a hand-held spirometer they have been provided with.
Baseline information, information at the time of RVI episode, and follow-up data will be collected standardized case report forms (CRF).
Status: The study is currently enrolling with more than 100 participants. It is also in the early analysis phase.
University of Washington Medical Center
Study Sites
St. Joseph’s Hospital and Medical Center
Washington University in St. Louis

